-
PDF
- Split View
-
Views
-
Cite
Cite
R. S. Hinman, K. M. Crossley, J. McConnell, K. L. Bennell, Does the application of tape influence quadriceps sensorimotor function in knee osteoarthritis?, Rheumatology, Volume 43, Issue 3, March 2004, Pages 331–336, https://doi.org/10.1093/rheumatology/keh033
Close - Share Icon Share
Abstract
Objectives. Using additional data from two previously reported studies, the aim was to determine the effects of immediate and short-term continuous (3 weeks) application of knee tape on quadriceps sensorimotor function in individuals with symptomatic knee osteoarthritis (OA).
Methods. A within-subjects study (n = 18) and a randomized controlled trial (n = 87) were performed using community volunteers. Therapeutic tape (patellar realignment and soft-tissue unloading) was compared with control (placebo) tape and no tape. Outcome measures included knee joint position sense, isometric quadriceps strength and electromyographic quadriceps onset during stair descent.
Results. Application of therapeutic tape worsened joint position sense (variable error) at a knee angle of 40° (P < 0.01), but did not immediately alter any other sensorimotor parameter. Even after 3 weeks of wearing tape continuously, sensorimotor function was not altered. Furthermore, no differential effect of tape was noted when participants were dichotomized into those with poor and good sensorimotor scores at baseline.
Conclusions. Neither immediate application nor continuous use of tape (for 3 weeks) appears to influence sensorimotor function in people with knee OA. Alterations in sensorimotor function cannot explain the pain-relieving effects of therapeutic tape observed in this population.
Patellar taping was developed as a physiotherapy treatment for patellofemoral pain syndrome (PFPS) [1]. Despite substantial evidence demonstrating tape's immediate pain-relieving effect [2–7], it remains unclear how this is achieved. Although postulated to improve patellar position, thus reducing patellofemoral joint (PFJ) stress and knee pain [1], evidence is conflicting as to whether a positional change occurs with taping [8]. It has been suggested that cutaneous and mechanical effects of tape may enhance sensorimotor variables, such as proprioceptive acuity, quadriceps strength and vastus medialis obliquus (VMO) onset [8]. Whilst PFPS studies demonstrate an immediate, positive effect of tape on quadriceps strength and VMO onset [3, 6, 7, 9–12], no study has investigated the effect of tape on proprioception in patients with knee pathology.
Knee taping is increasingly being used to manage other knee pain conditions. Contemporary studies by us and others demonstrate the efficacy of tape in reducing pain associated with knee osteoarthritis (OA) [13–15], yet even less is known about the mechanism underpinning its effects in this population compared with patients with PFPS. Does tape increase quadriceps strength in the osteoarthritic patient? Can it enhance variables related to onset of muscle activity and/or proprioception in knee OA? These questions remain unanswered. Individuals with knee OA demonstrate quadriceps weakness and impaired proprioceptive acuity compared with age-matched controls [16–21], providing ample opportunity for improvement with tape. Whilst a synchronous onset of VMO and vastus lateralis (VL) is evident in knee OA [22], patients do demonstrate a delayed global onset of quadriceps activity [23] that may be amenable to improvement with tape.
Quadriceps dysfunction may be important in the development and progression of structural change and pain associated with knee OA. Quadriceps weakness poses a risk for disease incidence [24] and determines both pain severity and disability in knee OA [20, 25–27]. Neuromuscular control is critical in attenuating ground-reaction forces and associated rates of loading during gait [28–30]. Quadriceps dysfunction may compromise protective mechanisms, leading to excessive joint movement and instability, and reduced shock absorption during gait, and ultimately joint pain. Thus, targeted interventions to improve quadriceps function are desirable for knee OA.
Our investigations demonstrate that therapeutic tape is efficacious for knee OA. Therapeutic tape immediately reduces pain by 40–50% on locomotion, a change greater than that observed with control (placebo) tape [14]. Furthermore, wearing tape for 3 weeks improves self-reported disability, and beneficial effects of tape on pain and disability persist after taping has ceased [13]. To evaluate mechanisms that may underpin these effects of tape, we collected additional data during our prior investigations. The present paper reports these secondary findings and aims to determine the effects of immediate and short-term continuous application of tape on quadriceps sensorimotor function in symptomatic knee OA.
Methods
Experiment A: immediate effects
This involved a within-subjects design. Sensorimotor function was assessed immediately following application of (i) therapeutic tape (designed to reduce pain), (ii) control tape (designed to approximate a placebo) and (iii) no tape. Order of testing was randomly assigned [31]. Eighteen participants (Table 1) aged over 50 yr with knee OA were recruited from the community. Diagnosis was based on American College of Rheumatology criteria [32]. Specific details regarding this cohort have been reported previously [14].
Participant characteristics for experiment A (cohort A) and experiment B (cohort B)
| . | Cohort A . | Cohort B . |
|---|---|---|
| . | (n = 18) . | (n = 87) . |
| Age (yr) | 67 (7) | 69 (9) |
| Male, female | 12, 6 | 57, 30 |
| Height (m) | 1.65 (0.10) | 1.64 (0.09) |
| Weight (kg) | 80 (11) | 80 (14) |
| Body mass index (kg/m2) | 29.4 (4.0) | 29.6 (4.3) |
| . | Cohort A . | Cohort B . |
|---|---|---|
| . | (n = 18) . | (n = 87) . |
| Age (yr) | 67 (7) | 69 (9) |
| Male, female | 12, 6 | 57, 30 |
| Height (m) | 1.65 (0.10) | 1.64 (0.09) |
| Weight (kg) | 80 (11) | 80 (14) |
| Body mass index (kg/m2) | 29.4 (4.0) | 29.6 (4.3) |
Values are mean (s.d.) unless otherwise stated.
Participant characteristics for experiment A (cohort A) and experiment B (cohort B)
| . | Cohort A . | Cohort B . |
|---|---|---|
| . | (n = 18) . | (n = 87) . |
| Age (yr) | 67 (7) | 69 (9) |
| Male, female | 12, 6 | 57, 30 |
| Height (m) | 1.65 (0.10) | 1.64 (0.09) |
| Weight (kg) | 80 (11) | 80 (14) |
| Body mass index (kg/m2) | 29.4 (4.0) | 29.6 (4.3) |
| . | Cohort A . | Cohort B . |
|---|---|---|
| . | (n = 18) . | (n = 87) . |
| Age (yr) | 67 (7) | 69 (9) |
| Male, female | 12, 6 | 57, 30 |
| Height (m) | 1.65 (0.10) | 1.64 (0.09) |
| Weight (kg) | 80 (11) | 80 (14) |
| Body mass index (kg/m2) | 29.4 (4.0) | 29.6 (4.3) |
Values are mean (s.d.) unless otherwise stated.
Experiment B: short-term effects
This involved a randomized controlled trial (RCT), in which 87 participants with knee OA (Table 1) were randomly allocated to receive 3 weeks of (i) therapeutic tape, (ii) control tape or (iii) no tape. Specific details regarding this trial have been reported [13]. Sensorimotor function was assessed at baseline and following the intervention (final assessment). For people allocated a taping intervention, assessment took place with the knee untaped.
Experiments were approved by the University of Melbourne Human Research Ethics Committee. All participants provided written informed consent.
Taping
Standardized procedures were followed [13, 14] by trained physiotherapists. Therapeutic tape [rigid strapping tape (Leuko Sportstape Premium Plus; Beiersdorf Australia) over hypoallergenic under-tape (Fixomull® stretch; North Rhyde, Beiersdorf Australia)] aimed to reposition the patella (medial glide and lateral and anteroposterior tilt) and to relieve strain on either the infrapatellar fat pad or the pes anserinus (unloading). Control taping involved applying hypoallergenic tape over the same areas of skin as would be covered by therapeutic tape and provided cutaneous input only. Participants were unaware which tape technique was considered therapeutic. For experiment B, tape was worn continuously and re-applied weekly.
Outcomes
Proprioception
Assessment of knee joint position sense (JPS) is an accepted indirect measure of proprioception [16, 17]. JPS was examined with the participant sitting, using an established protocol [33, 34]. Reflective markers were attached to the greater trochanter, iliotibial tract (at the superior border of the patella), neck of the fibula and lateral malleolus. With the participant's eyes closed, the knee was passively extended to one of two test positions (20° and 40° flexion). The participant then held the test position, ‘sensing’ the joint position. Upon return to the resting position, the participant was asked to extend the knee to the perceived test position (response position). Each test position was examined five times. Knee angles were calculated using computer analysis of videotape recordings and the two-dimensional automatic digitizing module of the Peak measurement system (Peak Motus [v4.3.1], Peak Performance Technologies Incorporated, Englewood, CO, USA). Two variables were calculated at each test angle: (i) absolute error (mean absolute difference between the five test and response positions irrespective of the sign of the difference), representing accuracy; and (ii) variable error [standard deviation from the mean of each set of five relative errors (arithmetic difference between test and response positions)], representing consistency.
Quadriceps strength
Isometric strength was assessed at 60° knee flexion using a KinCom isokinetic dynamometer (Chattexc Corporation, Chattanooga, TN, USA). Participants were secured and performed a submaximal warm-up for familiarization. Three maximal contractions of 5 s duration were performed, with 15 s rest between. Highest peak force was recorded and corrected for body weight.
Quadriceps onset
VL activity was recorded using surface electromyography (EMG) during five trials of stair descent (as VL is the predominant force producer [35]) [23, 36]. Data were telemetred, bandpass-filtered between 20 and 500 Hz, sampled at 1000 Hz and 12-bit A–D converted. Data were full-wave rectified and low-pass filtered at 50 Hz. Computer-identified muscle onsets were confirmed with visual analysis. Muscle onset was quantified by subtracting the time of foot contact (determined from video analysis) from the time of muscle onset. Negative onsets indicate muscle pre-activation. Results were averaged over five trials.
Data analysis
Experiment A
Outcomes were compared using a one-way repeated-measures analysis of variance (SPSS; Norusis/SPSS, Chicago, IL, USA). Post hoc paired t-tests were used to locate significant differences using a Bonferroni-adjusted α of 0.017.
Experiment B
Intervention effects were evaluated in each group by comparing baseline and final data using the Wilcoxon signed ranks test (adjusted α level of 0.01). Change in each variable was calculated by subtracting the baseline score from the final score. Change scores were compared with Kruskal–Wallis tests.
Secondary analyses determined if taping effects differed according to baseline sensorimotor impairment. For every variable, each taping group was dichotomized into those with ‘good’ and those with ‘poor’ baseline function (based on the median score across the cohort). Change in each outcome with tape was then compared between subgroups using Mann–Whitney U-tests (α level of 0.01).
Results
Joint position sense
Experiment A
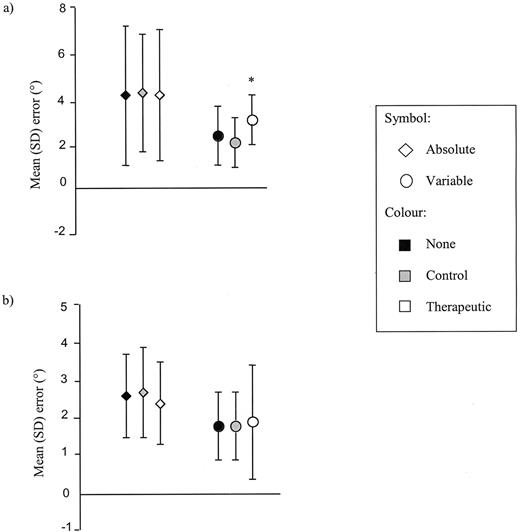
Mean (s.d.) absolute and variable error at 40° was 4.1 (3.1)° and 2.3 (1.3)° respectively with no tape. Whilst absolute error did not differ with the application of tape, variable error increased with therapeutic tape (P < 0.01) (Fig. 1a). Mean (s.d.) absolute and variable error at 20° was 2.6 (1.1)° and 1.8 (0.9)° respectively with no tape. Tape did not alter JPS at this position (Fig. 1b).
Immediate effect of tape on knee joint position sense error at a knee angle of (a) 40° and (b) 20° as observed in experiment A. Note that the shape of the symbol depicts the type of error, whilst its colour depicts the taping condition. The asterisk (*) indicates a significant difference from both other test conditions (P < 0.01).
Experiment B
JPS was unchanged following 3 weeks of either control or therapeutic tape (Table 2). Change in JPS was similar in all groups. There was no difference in change scores with therapeutic tape between individuals with good and poor JPS. However, control tape resulted in significantly greater improvement in variable error (40°) in those with poor JPS compared with those with good JPS (P < 0.01).
Effects of a 3-week application of knee tape on quadriceps sensorimotor function, as determined in experiment B
| . | No tape . | . | Control tape . | . | Therapeutic tape . | . | . |
|---|---|---|---|---|---|---|---|
| . | Baseline . | Final . | Baseline . | Final . | Baseline . | Final . | . |
| Variable . | (n = 29) . | (n = 28) . | (n = 29) . | (n = 29) . | (n = 29) . | (n = 29) . | P . |
| JPS error 40° | |||||||
| Absolute | 2.9 | 2.4 | 2.5 | 2.6 | 2.6 | 2.4 | 0.724 |
| (2.1, 3.5) | (2.0, 3.6) | (1.8, 3.9) | (1.8, 4.1) | (1.8, 3.3) | (1.8, 3.6) | ||
| Variable | 2.2 | 2.2 | 2.4 | 1.8 | 2.3 (1.6, 2.9) | 2.5 | 0.054 |
| (1.3, 2.9) | (1.1, 3.1) | (1.7, 3.0) | (1.5, 2.7) | (1.8, 3.1) | |||
| JPS error 20° | |||||||
| Absolute | 2.3 | 1.8 | 2.0 | 2.0 | 2.1 | 2.0 | 0.779 |
| (1.5, 2.9) | (1.4, 3.0) | (1.6, 2.6) | (1.5, 2.9) | (1.3, 2.8) | (1.1, 3.2) | ||
| Variable | 1.7 | 1.7 | 1.9 | 1.9 | 1.9 | 1.6 | 0.600 |
| (0.9, 2.6) | (1.0, 3.1) | (1.2, 2.2) | (1.3, 2.3) | (1.3, 2.7) | (1.2, 2.3) | ||
| Quad strength (N/kg) | 2.9 | 3.0 | 3.8 | 4.1 | 3.9 | 3.6 | 0.218 |
| (1.4, 4.5) | (1.4, 5.0) | (2.7, 4.8) | (2.5, 5.1) | (2.5, 4.7) | (2.6, 4.9) | ||
| Quad onset (ms) | −358 | −330 | −386 | −356 | −372 | −331 | 0.696 |
| (−474, −289) | (−464, −260) | (−505, −347) | (−473, −279) | (−486, −262) | (−463, −254) |
| . | No tape . | . | Control tape . | . | Therapeutic tape . | . | . |
|---|---|---|---|---|---|---|---|
| . | Baseline . | Final . | Baseline . | Final . | Baseline . | Final . | . |
| Variable . | (n = 29) . | (n = 28) . | (n = 29) . | (n = 29) . | (n = 29) . | (n = 29) . | P . |
| JPS error 40° | |||||||
| Absolute | 2.9 | 2.4 | 2.5 | 2.6 | 2.6 | 2.4 | 0.724 |
| (2.1, 3.5) | (2.0, 3.6) | (1.8, 3.9) | (1.8, 4.1) | (1.8, 3.3) | (1.8, 3.6) | ||
| Variable | 2.2 | 2.2 | 2.4 | 1.8 | 2.3 (1.6, 2.9) | 2.5 | 0.054 |
| (1.3, 2.9) | (1.1, 3.1) | (1.7, 3.0) | (1.5, 2.7) | (1.8, 3.1) | |||
| JPS error 20° | |||||||
| Absolute | 2.3 | 1.8 | 2.0 | 2.0 | 2.1 | 2.0 | 0.779 |
| (1.5, 2.9) | (1.4, 3.0) | (1.6, 2.6) | (1.5, 2.9) | (1.3, 2.8) | (1.1, 3.2) | ||
| Variable | 1.7 | 1.7 | 1.9 | 1.9 | 1.9 | 1.6 | 0.600 |
| (0.9, 2.6) | (1.0, 3.1) | (1.2, 2.2) | (1.3, 2.3) | (1.3, 2.7) | (1.2, 2.3) | ||
| Quad strength (N/kg) | 2.9 | 3.0 | 3.8 | 4.1 | 3.9 | 3.6 | 0.218 |
| (1.4, 4.5) | (1.4, 5.0) | (2.7, 4.8) | (2.5, 5.1) | (2.5, 4.7) | (2.6, 4.9) | ||
| Quad onset (ms) | −358 | −330 | −386 | −356 | −372 | −331 | 0.696 |
| (−474, −289) | (−464, −260) | (−505, −347) | (−473, −279) | (−486, −262) | (−463, −254) |
Data are median (interquartile range). There were no significant differences across time within the intervention groups.
*P values represent results of the between-group comparisons of change scores (Kruskal–Wallis test).
Quad, quadriceps.
Effects of a 3-week application of knee tape on quadriceps sensorimotor function, as determined in experiment B
| . | No tape . | . | Control tape . | . | Therapeutic tape . | . | . |
|---|---|---|---|---|---|---|---|
| . | Baseline . | Final . | Baseline . | Final . | Baseline . | Final . | . |
| Variable . | (n = 29) . | (n = 28) . | (n = 29) . | (n = 29) . | (n = 29) . | (n = 29) . | P . |
| JPS error 40° | |||||||
| Absolute | 2.9 | 2.4 | 2.5 | 2.6 | 2.6 | 2.4 | 0.724 |
| (2.1, 3.5) | (2.0, 3.6) | (1.8, 3.9) | (1.8, 4.1) | (1.8, 3.3) | (1.8, 3.6) | ||
| Variable | 2.2 | 2.2 | 2.4 | 1.8 | 2.3 (1.6, 2.9) | 2.5 | 0.054 |
| (1.3, 2.9) | (1.1, 3.1) | (1.7, 3.0) | (1.5, 2.7) | (1.8, 3.1) | |||
| JPS error 20° | |||||||
| Absolute | 2.3 | 1.8 | 2.0 | 2.0 | 2.1 | 2.0 | 0.779 |
| (1.5, 2.9) | (1.4, 3.0) | (1.6, 2.6) | (1.5, 2.9) | (1.3, 2.8) | (1.1, 3.2) | ||
| Variable | 1.7 | 1.7 | 1.9 | 1.9 | 1.9 | 1.6 | 0.600 |
| (0.9, 2.6) | (1.0, 3.1) | (1.2, 2.2) | (1.3, 2.3) | (1.3, 2.7) | (1.2, 2.3) | ||
| Quad strength (N/kg) | 2.9 | 3.0 | 3.8 | 4.1 | 3.9 | 3.6 | 0.218 |
| (1.4, 4.5) | (1.4, 5.0) | (2.7, 4.8) | (2.5, 5.1) | (2.5, 4.7) | (2.6, 4.9) | ||
| Quad onset (ms) | −358 | −330 | −386 | −356 | −372 | −331 | 0.696 |
| (−474, −289) | (−464, −260) | (−505, −347) | (−473, −279) | (−486, −262) | (−463, −254) |
| . | No tape . | . | Control tape . | . | Therapeutic tape . | . | . |
|---|---|---|---|---|---|---|---|
| . | Baseline . | Final . | Baseline . | Final . | Baseline . | Final . | . |
| Variable . | (n = 29) . | (n = 28) . | (n = 29) . | (n = 29) . | (n = 29) . | (n = 29) . | P . |
| JPS error 40° | |||||||
| Absolute | 2.9 | 2.4 | 2.5 | 2.6 | 2.6 | 2.4 | 0.724 |
| (2.1, 3.5) | (2.0, 3.6) | (1.8, 3.9) | (1.8, 4.1) | (1.8, 3.3) | (1.8, 3.6) | ||
| Variable | 2.2 | 2.2 | 2.4 | 1.8 | 2.3 (1.6, 2.9) | 2.5 | 0.054 |
| (1.3, 2.9) | (1.1, 3.1) | (1.7, 3.0) | (1.5, 2.7) | (1.8, 3.1) | |||
| JPS error 20° | |||||||
| Absolute | 2.3 | 1.8 | 2.0 | 2.0 | 2.1 | 2.0 | 0.779 |
| (1.5, 2.9) | (1.4, 3.0) | (1.6, 2.6) | (1.5, 2.9) | (1.3, 2.8) | (1.1, 3.2) | ||
| Variable | 1.7 | 1.7 | 1.9 | 1.9 | 1.9 | 1.6 | 0.600 |
| (0.9, 2.6) | (1.0, 3.1) | (1.2, 2.2) | (1.3, 2.3) | (1.3, 2.7) | (1.2, 2.3) | ||
| Quad strength (N/kg) | 2.9 | 3.0 | 3.8 | 4.1 | 3.9 | 3.6 | 0.218 |
| (1.4, 4.5) | (1.4, 5.0) | (2.7, 4.8) | (2.5, 5.1) | (2.5, 4.7) | (2.6, 4.9) | ||
| Quad onset (ms) | −358 | −330 | −386 | −356 | −372 | −331 | 0.696 |
| (−474, −289) | (−464, −260) | (−505, −347) | (−473, −279) | (−486, −262) | (−463, −254) |
Data are median (interquartile range). There were no significant differences across time within the intervention groups.
*P values represent results of the between-group comparisons of change scores (Kruskal–Wallis test).
Quad, quadriceps.
Quadriceps strength
Experiment A
Mean (s.d.) strength was 3.70 (1.57) N/kg for the no-tape condition. Tape application did not immediately alter strength.
Experiment B
Strength was unchanged following 3 weeks of knee tape (Table 2). No differences in change in strength were evident between groups. Similarly, no differences in change scores were evident comparing those with poor and good baseline strength, with either taping technique.
Quadriceps onset
Experiment A
Mean (s.d.) quadriceps onset was 409 (150) ms prior to foot-contact for the no tape condition. Tape did not alter this variable.
Experiment B
A 3-week application of tape did not alter quadriceps onset (Table 2). Similar changes were observed between the three groups. No differences were detected in change scores between those with ‘good’ (i.e. earlier) onset and those with ‘poor’ (i.e. later) onset with either tape technique.
Discussion
This is the first investigation evaluating knee tape and quadriceps sensorimotor function in OA. The efficacy of therapeutic tape in reducing pain in knee OA has been demonstrated [13–15]. However, results of this study show that tape generally does not influence sensorimotor variables in this population, either immediately upon application or after 3 weeks of continuous wear.
Our knee OA results differ from similar studies in healthy and PFPS cohorts. Current evidence strongly suggests that tape increases quadriceps strength in PFPS [6, 7, 9–11]. It is unknown how this is achieved, but placebo-controlled studies have excluded enhanced cutaneous stimulation as a mechanism [7, 11]. A mechanical effect of tape on the quadriceps lever is possible. Reduced inhibition, due to concomitant pain relief, is another explanation. It is unclear why strength was unchanged with tape in knee OA. Pain relief achieved with tape may not be large enough for strength to be improved in this population. However, this is unlikely given that pain reductions are comparable to those observed in PFPS. The multifactorial nature of quadriceps weakness in knee OA is a possible explanation. Muscle weakness may be attributed to arthrogenous inhibition [37, 38], muscle fibre atrophy or myopathic change [39, 40]. It is not physiologically possible for tape to reverse these latter factors.
Only one study has evaluated tape's effects on knee proprioception [41]. In 52 healthy volunteers, and using a taping procedure similar to our control tape, no change in JPS was demonstrated. However, when participants with good and poor proprioception were compared, taping improved poor proprioceptive acuity, suggesting that tape only benefits individuals with poor acuity at the outset. Proprioceptive deficits are associated with knee OA [16, 18, 19, 42]; thus it is somewhat surprising that we did not observe beneficial effects of tape on proprioception in our experiments. However, our finding of improved variable error (40°) with control tape in those with poor JPS supports Callaghan et al. [41]. In contrast, therapeutic tape immediately worsened JPS (variable error at 40°). As this variable was unaltered after 3 weeks of taping, this suggests that the negative influence occurs only whilst tape is in situ. Immediate, increased input from cutaneous afferents, triggered by contact and movement of rigid tape on the skin, may ‘confuse’ the nervous system, rather than enhance, and may explain the greater inconsistency in JPS observed at 40° with therapeutic tape.
Conflicting findings are reported about external knee supports and proprioception in OA. Whilst Barrett et al. [43] reported improved JPS with elastic bandaging, two subsequent studies failed to support these findings [16, 44]. Similar to our results, those of Hassan et al. [44] reported worsening of JPS with a standard-sized elastic bandage in 68 people with knee OA. In individuals with medial OA and varus malalignment, custom-fit valgus braces improve JPS [45], possibly due to improved joint alignment or unloading of the medial compartment. Given that muscle receptors play a primary role in mediating proprioceptive information [46] and the relatively small area of skin covered by tape, it is probable that enhanced cutaneous sensation with tape is insufficient to result in positive changes in JPS.
Contrary to PFPS [3, 12], quadriceps onset was unaffected by taping the knee, which may be related to the non-significant effect on proprioception. Pain inhibits quadriceps activity [47, 48]; thus, an earlier onset of activity was anticipated with reduced pain following taping. Despite immediate and sustained pain relief with therapeutic tape, muscle onset was unchanged. It is possible that factors other than pain inhibition, and not amenable to change with tape, contribute to the delayed quadriceps onset in OA [23].
As sample sizes were determined using pain as the primary outcome, there is a risk that participant numbers were inadequate to detect differences in sensorimotor variables. However, changes after 3 weeks of taping were quite small (Table 2) and similar to those observed with no tape. It is unlikely that these changes were related to knee tape application, so increased participant numbers would be of little value.
Mechanisms responsible for pain relief with tape in knee OA are unclear. However, this study suggests that altered sensorimotor function does not play a major role. We propose that pain relief is achieved primarily by tape's mechanical influence on patellar position. The PFJ is commonly involved in knee OA [49–51], with the lateral compartment predominantly affected [52, 53]. Radiographic PFJ OA has been correlated with patellar malalignment [54]. We hypothesize that taping unloads the lateral facet, leading to reduced, or redistributed, contact pressures. Pain relief is also probably achieved by unloading painful, inflamed soft tissues, such as the infrapatellar fat pad. A small placebo effect is also likely with more prolonged applications.
Knee tape does not appear to be useful for enhancing quadriceps sensorimotor function in symptomatic knee OA. Whilst beneficial for pain relief, other interventions, such as strengthening exercises, balance activities and functional retraining, may be more appropriate in reversing sensorimotor deficits. However, due to its pain-relieving effects, tape used in conjunction with exercise interventions may maximize participation, resulting in greater sensorimotor improvements than may be observed with exercise alone.
The authors wish to thank Dr Mike Smith for evaluation of radiographs, Drs Sallie Cowan and Barry Stillman for technical and scientific advice and the project physiotherapists for their assistance in performing the taping interventions in experiment B. These experiments were supported by funding from the National Health and Medical Research Council (Grant 114277), the ANZ Charitable Trusts, the Australian Physiotherapy Association and the Arthritis Foundation of Australia.
References
McConnell JS. The management of chondromalacia patellae: a long term solution.
Salsich G, Brechter J, Farwell D, Powers C. The effects of patellar taping on knee kinetics, kinematics, and vastus lateralis muscle activity during stair ambulation in individuals with patellofemoral pain.
Cowan SM, Bennell KL, Hodges PW. Therapeutic patellar taping changes the timing of vasti muscle activation in people with patellofemoral pain syndrome.
Powers CM, Landel R, Sosnick T et al. The effects of patellar taping on stride characteristics and joint motion in subjects with patellofemoral pain.
Bockrath K, Wooden C, Worrell T, Ingersoll CD, Farr J. Effects of patella taping on patella position and perceived pain.
Conway A, Malone TR, Conway P. Patella alignment/tracking alteration: effect of force output and perceived pain.
Handfield T, Kramer J. Effect of McConnell taping on perceived pain and knee extensor torques during isokinetic exercise performed by patients with patellofemoral pain syndrome.
Crossley K, Cowan SM, Bennell KL, McConnell J. Patellar taping: is clinical success supported by scientific evidence?
Werner S, Knutsson E, Eriksson E. Effect of taping the patella on concentric and eccentric torque and EMG of knee extensor and flexor muscles in patients with patellofemoral pain syndrome.
Herrington L. The effect of patellar taping on quadriceps peak torque and perceived pain: a preliminary study.
Ernst GP, Kawaguchi J, Saliba E. Effect of patellar taping on knee kinetics of patients with patellofemoral pain syndrome.
Gilleard W, McConnell J, Parsons D. The effect of patellar taping on the onset of vastus medialis obliquus and vastus lateralis muscle activity in persons with patellofemoral pain.
Hinman R, Crossley K, McConnell J, Bennell K. Efficacy of knee tape in the management of knee osteoarthritis: a blinded randomised controlled trial.
Hinman R, Bennell K, Crossley K, McConnell J. Immediate effects of adhesive tape on pain and disability in individuals with knee osteoarthritis.
Cushnaghan J, McCarthy C, Dieppe P. Taping the patella medially: a new treatment for osteoarthritis of the knee joint?
Hewitt B, Refshauge K, Kilbreath S. Kinesthesia at the knee: the effect of osteoarthritis and bandage application.
Barrack RL, Skinner HB, Cook SD, Haddad RJ Jr. Effect of articular disease and total knee arthroplasty on knee joint position sense.
Pai Y-C, Rymer WZ, Chang RW, Sharma L. Effect of age and osteoarthritis on knee proprioception.
Hassan B, Mockett S, Doherty M. Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects.
Slemenda C, Brandt KD, Heilman DK et al. Quadriceps weakness and osteoarthritis of the knee.
Hurley MV, Scott DL, Rees J, Newham DJ. Sensorimotor changes and functional performance in patients with knee osteoarthritis.
Hinman R, Bennell K, Metcalf B, Crossley K. Temporal activity of vastus medialis obliquus and vastus lateralis in symptomatic knee osteoarthritis.
Hinman RS, Bennell KL, Metcalf BR, Crossley KM. Delayed onset of quadriceps activity and altered knee joint kinematics during stair stepping in individuals with knee osteoarthritis.
Slemenda C, Heilman D, Brandt K et al. Reduced quadriceps strength relative to body weight: a risk factor for knee osteoarthritis in women?
O’Reilly SC, Jones A, Muir KR, Doherty M. Quadriceps weakness in knee osteoarthritis: the effect on pain and disability.
McAlindon TE, Cooper C, Kirwan JR, Dieppe PA. Determinants of disability in osteoarthritis of the knee.
van Baar ME, Dekker J, Lemmens JAM, Oostendorp RAB, Bijlsma JWJ. Pain and disability in patients with osteoarthritis of hip or knee: the relationship with articular, kinesiological, and psychological characteristics.
Jefferson RJ, Collins JJ, Whittle MW, Radin EL, O’Connor JJ. The role of the quadriceps in controlling impulsive forces around heelstrike.
Portney L, Watkins M. Foundations of clinical research. Applications to practice, 2nd ed. Upper Saddle River, NJ: Prentice Hall Health,
Altman R, Asch E, Bloch D et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee.
Bennell K, Hinman R, Metcalf B et al. Relationship of knee joint proprioception to pain and disability in individuals with knee osteoarthritis.
Stillman B, Tully E, McMeeken J. Knee joint mobility and position sense in healthy young adults.
McFadyen BJ, Winter DA. An integrated biomechanics analysis of normal stair ascent and descent.
Cowan SM, Bennell KL, Hodges PW. The test–retest reliability of the onset of concentric and eccentric vastus medialis obliquus and vastus lateralis electromyographic activity in a stair stepping task.
Hurley MV. The effects of joint damage on muscle function, proprioception and rehabilitation.
Glasberg MR, Glasberg JR, Jones RE. Muscle pathology in total knee replacement for severe osteoarthritis.
Nakamura T, Suzuki K. Muscular changes in osteoarthritis of the hip and knee.
Callaghan M, Selfe J, Bagley P, Oldham J. The effects of patellar taping on knee joint proprioception.
Sharma L, Pai Y-C, Holtkamp K, Rymer WZ. Is knee joint proprioception worse in the arthritic knee versus the unaffected knee in unilateral knee osteoarthritis?
Barrett DS, Cobb AG, Bentley G. Joint proprioception in normal, osteoarthritic and replaced knees.
Hassan B, Mockett S, Doherty M. Influence of elastic bandage on knee pain, proprioception, and postural sway in subjects with knee osteoarthritis.
Birmingham T, Kramer J, Kirkley A, Ingliss J, Spaulding S, Vandervoort A. Knee bracing for medial compartment osteoarthritis: effects on proprioception and postural control.
Johansson HS, Jolander P.
Arvidsson I, Eriksson E, Knutsson ESA, Arner S. Reduction of pain inhibition on voluntary muscle activation by epidural analgesis.
Hassan B, Doherty S, Mockett S, Doherty M. Effect of pain reduction on postural sway, proprioception, and quadriceps strength in subjects with knee osteoarthritis.
Ledingham J, Regan M, Jones A, Doherty M. Radiographic patterns and associations of osteoarthritis of the knee in patients referred to hospital.
McAlindon TE, Snow S, Cooper C, Dieppe PA. Radiographic patterns of osteoarthritis of the knee joint in the community: the importance of the patellofemoral joint.
Davies A, Vince A, Shepstone L, Donell S, Glasgow M. The radiologic prevalence of patellofemoral osteoarthritis.
Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y. Roentographic and clinical findings of patellofemoral arthritis.
Elahi S, Cahue S, Felson DT, Engelman L, Sharma L. The association between varus–valgus alignment and patellofemoral osteoarthritis.
Author notes
1Centre for Sports Medicine Research and Education, School of Physiotherapy, University of Melbourne, Victoria and 2McConnell and Clements Physiotherapy, Mosman, NSW, Australia.



Comments